Inteleos Blog: Case of the Quarter
 Author:
Author:
Falguni Patel (BS,RDMS,RVT,RMSKS)
Falu is an advanced pediatric sonographer at Lurie Children’s Hospital of Chicago for over twenty years. She is credentialed by the American Registry of Diagnostic Medical Sonography in Abdomen, Obstetrical and Gynecological, Neurosonology, Pediatric, Vascular Technology, and Musculoskeletal specialties. She serves on the Contrast, Musculoskeletal and Pediatric Imaging committee.
Patient History: 11-year-old male with abdominal pain, fever and vomiting for three days.
Clinical Information: Pain in the Right Lower Quadrant. (RLQ)
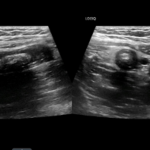
Figure 1. Mid-longitudinal view of the appendix (left) and transverse view of the appendix.
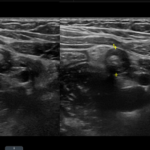
Figure 2. Transverse view of the appendix. The diameter of the appendix is 1.14 cm. Appendix diameter of >0.6 cm in the dilated segment is consistent with appendicitis.
Figure 3. A small appendicolith was also seen within the lumen of the appendix.
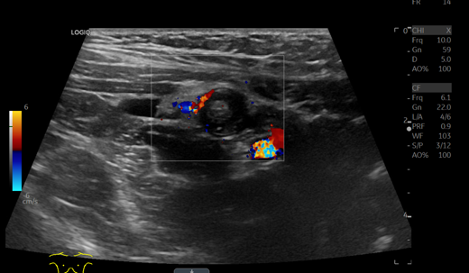
Figure 4. Color Doppler shows increased vascularity suggestive of mural hyperemia. A small amount of periappendiceal fluid was seen (yellow arrow). The iliac vessels and also seen in the right lower region of the color box.
In the above images (Figures 1- 4) of right lower quadrant, there is a dilated, blind ending tubular structure most consistent with an enlarged appendix.
Appendix size:
The appendix is dilated, measuring 1.14 cm in outer diameter (outer wall to outer wall).
Compressibility of the appendix:
The appendix was noncompressible and patient experienced excruciating pain during compression with the transducer.
Vascularity of the appendix:
Mild hyperemia.
Appendicolith:
A round, echogenic structure with posterior shadowing was seen within the lumen of the appendix, most consistent with appendicolith. The appendicolith measures approximately 0.5 x 0.7 x 0.2 cm.
Perforation:
No focal defect or a local collection was observed to suggest perforation was observed.
Abscess:
No abscess/ complex collection was seen in the region of the appendix. A small amount of periappendiceal fluid was seen.
Periappendiceal fat infiltration:
Increased echogenicity of fat tissue surrounding the appendix is due to periappendiceal fat infiltration.
Right lower quadrant transducer tenderness:
Patient reported marked tenderness with compression.
Periappendiceal fluid:
A small amount periappendiceal fluid was seen.
Adjacent bowel loops:
Unremarkable
IMPRESSION:
Acute appendicitis with appendicolith. Small volume of pelvic free fluid seen with no evidence of perforation of the appendix or periappendiceal abscess.
Take away points from the above case:
Remember to perform postvoid prior to scanning for appendix if the bladder is distended.
Remember to use a high frequency Linear transducer for better resolution.
Lateral approach and pelvic scanning in addition to the RLQ, may be useful.
Use posterior manual compression when performing graded compression to identify the appendix.
Remember to always document secondary signs when evaluating for appendicitis.
List of secondary signs to document when scanning for Appendicitis:
- Transverse AP measurement of greater 6mm
- Non compressible appendix
- Increased vascularity of appendix
- Absent vascularity of appendix in case of necrosis of the appendix
- Appendicolith
- Perforation
- Abscess
- Periappendiceal fat infiltration (hyperechoic fat)
- Periappendiceal fluid
- Adjacent bowel loop peristalsis
- Patient tenderness
Differential Diagnosis:
- Intussusception
- Meckel diverticulum
- Testicular torsion
- Kidney stones
- Viral and bacterial gastroenteritis
- PID
- Ovarian Torsion (female patient)
Complications for Appendicitis:
- Perforation
- Shock
- Pelvic abscess
- Wound infection
- Bowel obstruction